If you have acne, you can rest assured that you are not alone. It is one of the most common skin conditions worldwide. What is acne? In this blog, we will dive deeper into what acne is and how it is caused. At the end of the blog, you should better understand what type of acne you have.
-
 Dalacin-T LotionPrice range: £25.99 through £70.99
Dalacin-T LotionPrice range: £25.99 through £70.99 -
 Acnecide Gel (60g)Price range: £17.99 through £33.98
Acnecide Gel (60g)Price range: £17.99 through £33.98 -
 Duac 5 % Gel (30g)Price range: £22.99 through £59.97
Duac 5 % Gel (30g)Price range: £22.99 through £59.97
How common is acne?
The Global Burden of Disease Study 2010 identified acne vulgaris (commonly referred to as acne) as the eighth most common skin condition, affecting approximately 9.38% of people worldwide across all age groups.[1]
The prevalence of acne varies by country and age group, with studies estimating that between 35% and nearly 100% of adolescents experience acne at some point.[2]
What causes acne?
Acne is one of the most common skin conditions caused by small blockages of oil in the hair follicle.
There are four key components in the formation of acne:
These four components usually work together to cause acne. However, not all may be present, and they don’t have to occur in the same order.
Hormone sensitivity
Adolescence is a time when hormones run wild all over the body. The transition to adulthood has this intermediate stage where the body has to adjust to the influx of these hormones.
Acne is caused by sensitivity to normal levels of male hormones in the body.
Both men and women have male and female sex hormones, testosterone and oestrogen, in their bodies. Oestrogen is made from testosterone, and this conversion mainly occurs in the fat tissues. Look at the chemical structure of both below, and you will see how similar they are. See if you can spot the difference.
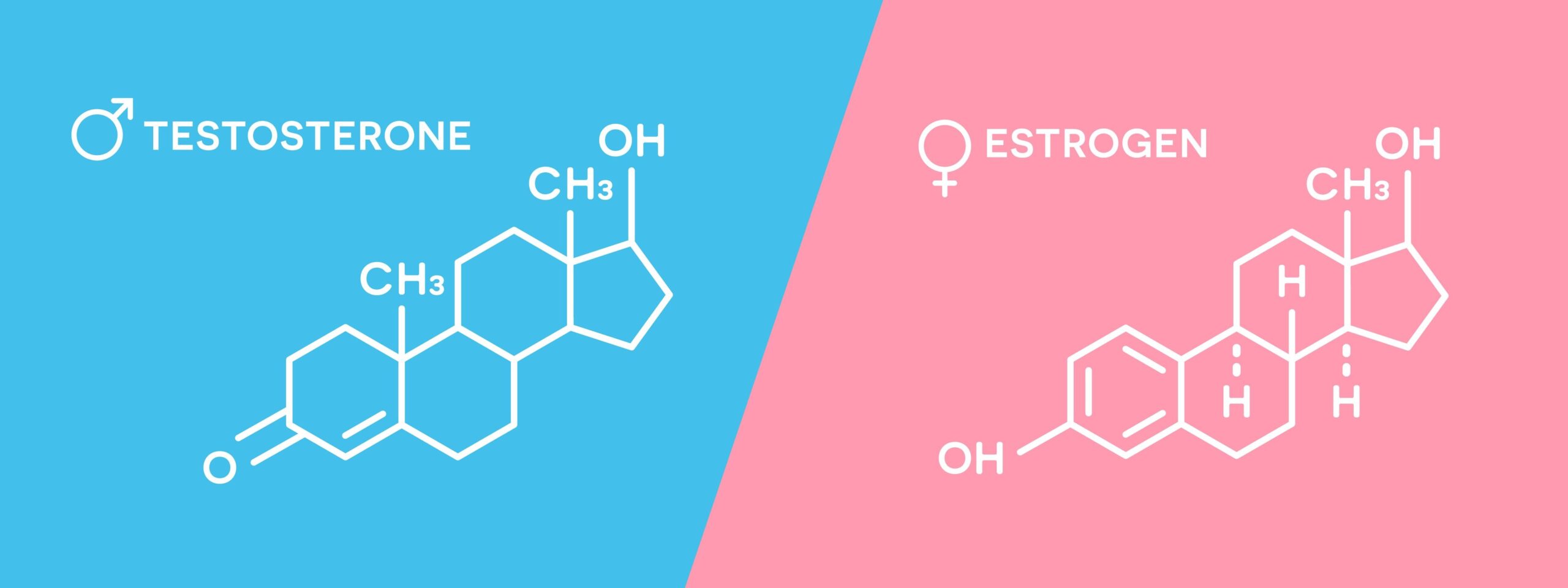
However, the male testosterone hormone is responsible for increased oil production on our skin. The reason for this increased sensitivity is unclear, but it is thought to be caused by increased hormone production during puberty.
More testosterone, more acne
Since boys have greater quantities of testosterone, this explains why boys usually have more severe forms of acne than girls.
Sticky sebum
Sebum is another name for the oil or grease on our skin. Excess sebum is triggered by testosterone and gives the skin a shiny appearance.
In people with acne, there is not only more sebum, but the quality of the sebum they produce is different; it’s thicker. So imagine if this thick, sticky, gloopy substance is pouring out of your skin; what will happen? Yes, things are going to stick to it.
People with acne also tend to have larger sebaceous glands, which are the factories where sebum is produced, than people without acne. This explains the problem of excess sebum.
Abnormal cell growth
At the same time, sebum production is increasing, and skin turnover is declining. The skin usually sheds dead skin, but when this process slows down, it becomes one of the acne triggers.
Skin cell lifecycle
All skin cells begin life at the bottom layer of the skin, called the dermis. Just like the sebaceous gland was the factory for producing sebum, the dermis is the factory for producing skin cells.
These newly born skin cells start to mature and then leave home like any young and maturing adult. The skin cells then make their way to the epidermis, the upper layer of skin. However, as they get nearer to the top of the skin layer, they start to die off. At the very top layers, they are shed with the everyday activities we carry out, like washing, scratching and putting on make-up.
When abnormal cell production occurs, in addition to being shed more slowly, more skin cells are produced than normal skin. So, this combination of reduced shedding and increased production helps tip the balance towards an environment more favourable to acne.
Blockage of hair follicles
Again, when dealing with the human body, we must learn the lessons of a famous childhood story, Goldilocks and the Three Bears. Just like Goldilocks preferred warm porridge over hot and cold porridge, our body always prefers the middle option: not too hot or cold. In the case of skin cells, it’s not too much or too little, but somewhere in between is the sweet spot for healthy skin.
When not enough skin cells are being shed, we have a recipe for disaster. These excess skin cells can then start to block the hair follicles.
What are hair follicles?
The follicles are the part of the skin that contains the hair. Remember the oil or sebum-producing factory, the sebaceous gland? This gland is attached to the hair follicle, releasing the oil it produces, which then escapes through the hair follicle and onto the skin’s surface.
Microcomedos
Doctors have named these blockages of the hair follicles by the excess dead skin cells microcomedos [6], and they are the starting point for acne.
So, imagine what happens when the hair follicle is blocked. The message that the hair follicle is blocked doesn’t reach the sebaceous gland, which continues to churn out sebum. Since a ‘plug’ has been formed by these dead skin cells, the oil has nowhere to go since its escape route out of the follicle has been effectively blocked.
This blockage can result in either:
- The oil behind the blockage becomes solid (like solidified fat) and, remains in the sebaceous gland, and does nothing or
- This greasy oil starts attracting bacteria, who love a fry-up.
Blackheads
When the blockage remains in a solid form, it can appear on the skin in two ways. The first is when the blockage of dead skin cells reaches the very top of the hair follicle and comes into contact with the air, which causes it to turn dark brown or black. It is thought that an oxidation process causes the colour change, much like when metal rusts and changes colour. This is an example of a classic “blackhead”.
Whiteheads
On the other hand, if the blockage is further down within the follicle, just below the surface, it will raise the skin as a bump. When this happens, we refer to it as a whitehead.
Non-inflammatory acne
What we have just described is known as non-inflammatory acne. We will now focus on what happens when the immune system gets involved, which naturally brings us to another acne trigger: bacteria.
Bacteria
We mentioned that both whiteheads and blackheads are examples of non-inflammatory acne. So, what causes inflammation? Let’s dive a bit deeper to find out.
When the skin becomes inflamed, the same processes occur: the small blockage caused by excess dead skin cells and sebum causing the blockage. However, when the oil is trapped within the follicle with nowhere to go, it’s like an all-you-can-eat buffet for bacteria.
Cutibacterium acnes
One bacteria is especially fond of a fry-up. It’s called Cutibacterium acnes, which is a bit of a mouthful, so we shorten it to C acnes.
These bacteria usually live on our skin and do not cause any problems, but again, remember the Goldilocks principle: for harmony, things have to be just right. So, when the conditions become favourable to the bacteria, they exploit this good fortune and start to multiply.
The C acnes bacteria is very adaptable. It can grow in conditions with little or no oxygen, such as a blocked hair follicle, or with plenty of oxygen on the skin.
Inflammation
When these bacteria start feasting, they are like rampaging hooligans. Given the right environment, all social contracts between humans and bacteria are broken in their quest to devour the nutritious detritus in the blocked follicle. In their feasting and multiplying, they damage their surroundings, rupturing follicles. The body responds to the assault on the trapped follicles by sending in its police officers, the white blood cells, to contain and eradicate the bacteria.
To the external eye, we know that this battle between the white blood cells and the bacteria is occurring because we start to see all the characteristic colours of a classic spot: yellow from the infection and red from the inflammation.
Inflammatory acne
The spot may be small or even fairly large; in some cases, the acne may be widespread and very deep. These lesions are known as inflammatory acne.
Treatments for acne
Several treatments are available for acne, and some contain a combination of ingredients to tackle different acne triggers. Here is a breakdown of the acne treatments at Medical Mojo:
- Acnecide – contains benzyl peroxide, kills bacteria and is an exfoliative
- Dalacin T topical lotion– antibiotic lotion which kills the bacteria
- Differin cream– contains adapalene, a form of vitamin A which reduces excess dead skin cells
- Duac gel– contains the antibiotic clindamycin and benzoyl peroxide, kills bacteria and exfoliates
- Epiduo gel– contains adapalene and benzoyl peroxide
- Lymecycline– an antibiotic
- Skinoren– contains azelaic acid, which reduces dead skin cells or keratin
- Tetralysal– contains the antibiotic lymecycline
- Treclin gel– contains clindamycin, an antibiotic, and tretinoin, a form of vitamin A that increases skin turnover.
- Zindaclin gel– contains clindamycin, an antibiotic.
-
 Treclin GelPrice range: £36.99 through £95.99
Treclin GelPrice range: £36.99 through £95.99 -
 Differin 0.1% CreamPrice range: £29.95 through £77.85
Differin 0.1% CreamPrice range: £29.95 through £77.85 -
 Skinoren 20% CreamPrice range: £19.99 through £50.97
Skinoren 20% CreamPrice range: £19.99 through £50.97
Summary
The picture is not quite black and white. People don’t have non-inflammatory or inflammatory acne, but usually, it’s a mixture of the two, with some people more prone to one or the other.
Some dermatologists advise always treating non-inflammatory acne to prevent it from progressing to more severe inflammatory acne.
A study found that 50 % of papules (red spots) started as normal-looking skin, although it’s possible a very tiny microcomedone may have been present. While 25% came from a whitehead (closed comedone), the remaining 25% came from a blackhead (an open comedone).
What to do now?
If you are unsure of what acne treatment is right for you, please contact us, and one of our prescribers will discuss the best options with you.
Alternatively, you can start the online acne consultation.
Disclaimer: This information is for educational purposes only and is not a replacement for professional medical advice.
References
- Vos, T. et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 380(9859), 2163–96
- Stathakis, V., Kilkenny, M. & Marks, R. Descriptive epidemiology of acne vulgaris in the community. Australas J Dermatol. 38(3), 115–23, https://doi.org/10.1111/j.1440-0960.1997.tb01126.x (1997).
- Gollnick HP, Zouboulis CC, Akamatsu H. Pathogenesis and pathogenesis related treatment of acne. J Dermatol. 1991 Sep;18(9):489-99.
- Cunliffe WJ, Holland DB, Clark SM, et al. Comedogenesis: some new aetiological, clinical, and therapeutic strategies. Dermatology. 2003;206(1):11-6.
- Corvec S, Dagnelie MA, Khammari A, et al. Taxonomy and phylogeny of cutibacterium (formerly propionibacterium) acnes in inflammatory skin diseases. Ann Dermatol Venereol. 2019 Jan;146(1):26-30.
- Knutson DD. Ultrastructural observations in acne vulgaris: the normal sebaceous follicle and acne lesions. J Invest Dermatol. 1974 Mar;62:288-307.
Are weight loss treatments making you tired, or have they led to a sudden increase in hair loss? Do you struggle with sleep?
Get a free month’s supply of one of our compounded treatments for energy, hair loss or sleep, with your first purchase of Mounjaro or Wegovy from Medical Mojo.
Claim your FREE offer