In the UK, the treatment of menopause can be generally managed by GPs. However, the same cannot be said when men experience symptoms of low testosterone due to andropause or late-onset hypogonadism. Both involve reductions in essential hormones as we age; the difference is that one hormone is oestrogen, while the other is the dreaded testosterone.
-
 Sildenafil 100mg Tablets£9.99 – £31.99
Sildenafil 100mg Tablets£9.99 – £31.99 -
 Sildenafil 50mg Tablets£7.99 – £31.99
Sildenafil 50mg Tablets£7.99 – £31.99 -
 Sildenafil 25mg Tablets£5.99 – £21.99
Sildenafil 25mg Tablets£5.99 – £21.99
What is TRT?
Testosterone Replacement Therapy (TRT) is a treatment used to help men with low levels of testosterone, a hormone that plays a key role in mood, energy, and overall health.
As men age, their testosterone levels naturally decrease, which can lead to symptoms like fatigue, depression, and reduced muscle mass.
TRT involves giving testosterone through injections or creams to bring levels back to normal and improve these symptoms.
To learn more about TRT, read our blog: What is TRT?
The stigma of testosterone
Unfortunately, testosterone has the disadvantage in that it comes with so much additional negative baggage. The media has stockpiled many clichés as a substitute for real journalism, for example, “testosterone-poisoned dictator”, “testosterone-fuelled rage”, and “roid rage”. The mere mention of the word “testosterone” sends a shiver down the spine of the chattering classes.
Toxic masculinity
In this day and age, in the era of toxic masculinity, the vilification of testosterone has been made easier.
Everything from wars to corporate greed has been blamed on testosterone. This may seem like reductionism in the extreme, but if the fault lies with the patriarchal society, then the fault must also lie with what makes man a man: testosterone.
However, leaving the current zeitgeist aside, the actual scientific data tells a different story. Numerous studies have demonstrated that the association of testosterone with violence and aggression is unwarranted. [1]
Why does your GP not prescribe TRT?
So why is there a difference in treating hormonal imbalances between men and women? Is there some form of gender discrimination at play here?
The current logic of the NHS is to allow GPs to initiate HRT for women suffering menopausal symptoms. At the same time, TRT can only be prescribed on the NHS if initiated in secondary or tertiary care settings.
This is because TRT is classed as an “amber” drug.[2]
NHS jargon
Before we go on, I will briefly explain some terminology to help you understand the NHS jargon.
When we talk about primary care, what do we mean?
Primary Care
Primary care refers to services that a person usually first sees when they have a health problem. For many people, this is often a GP or the practice nurse.
Primary care is based on caring for the person rather than specific conditions, so primary care professionals are generalists rather than specialists in any particular disease area.
Secondary Care
Secondary care services are usually based in a hospital or a clinic and include planned operations and specialist clinics such as cardiology or renal clinics.
Tertiary Care
Tertiary care is healthcare provided in more specialist centres.
Traffic Lights in the NHS
What do we mean when we say that TRT treatments are classified as “amber drugs”?
The Red Amber Green (RAG) classification offers guidance on the prescribing of drugs initiated in secondary care and reinforces the basic premise that:
“When clinical and/or prescribing responsibility for a patient is transferred from secondary to primary care, the primary care prescriber should have the appropriate competence to prescribe the necessary medicines. Therefore, it is essential that a transfer of care involving medicines that a primary care prescriber would not normally be familiar with should not take place without the sharing of information
with the primary care prescriber and their mutual agreement to the transfer of care.” [3]
This traffic light system aims to define where responsibility for prescribing should lie between primary and secondary care by categorising individual drugs as red, amber, or green.
Red
– for secondary or tertiary care initiation and long-term maintenance of prescribing
Amber
– drugs which are appropriate to be initiated and stabilised by a specialist in secondary or tertiary care; once stabilised, the drug may be appropriate for responsibility to be transferred from secondary to primary care with the agreement of a GP and a formal ‘shared care’ agreement.
Green (following specialist initiation)
– for drugs that must be initiated in secondary care but can then be safely prescribed in primary care with very little or no monitoring required.
Green (following specialist recommendation)
– Drugs that can be initiated by primary care following written or verbal advice from a specialist can then be safely prescribed in primary care with little or no monitoring.
Green
– drugs which may be initiated, stabilised and maintained in primary, secondary or tertiary care.
The demonisation of testosterone
So, now that the definitions are out of the way, let’s return to the demonisation of men.
What has led to this strange gender discrimination?
Late-onset hypogonadism or “andropause” is not a new phenomenon, and whilst in the past, men have been suffering in silence, more and more men are now making their voices heard.
Usually, men will have to do their own research before approaching their GP to ask about TRT. However, after clearing the first hurdle of getting past the receptionist, the obstacles to TRT only increase until they find themselves gridlocked by the above-mentioned traffic light system.
Referrals to secondary care
Once the GP is convinced that the symptoms are due to low testosterone, a referral needs to be made to a specialist clinic. Letters and emails are sent, and after much toing and froing, the Holy Grail of TRT may be obtained. But the time it takes to get the TRT on the NHS will probably test the patience of a saint.
However, while GPs regularly initiate and monitor HRT in females, local NHS Guidelines require them to refer male patients to secondary care for HRT initiation.

Late-onset hypogonadism
Even though late-onset hypogonadism is relatively common, it is often undiagnosed and untreated. [4]
This can be caused by many factors, one of which is that the symptoms of low testosterone mirror those from other comorbidities (such as obesity, hypertension, hyperlipidaemia, diabetes, erectile dysfunction, and depression).
In fact, the above-mentioned comorbidities are more common in hypogonadal men than in eugonadal ( normal testosterone levels) men. [5]
Viagra the quick fix
Time is another factor. Erectile dysfunction can quickly be addressed with phosphodiesterase five inhibitors such as that famous little blue pill, Viagra.
It’s a quick fix for a man complaining of erectile dysfunction in a ten-minute consultation but may do little to solve the underlying issue.
Many symptoms of erectile dysfunction can be signs of low testosterone, but it’s far easier to pop a pill than investigate root causes.
-
 Tadalafil 20mg tablets£8.99 – £32.99
Tadalafil 20mg tablets£8.99 – £32.99 -
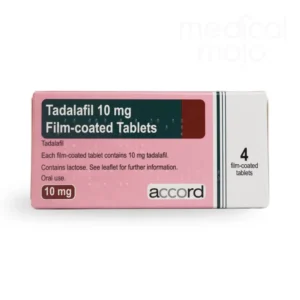 Tadalafil 10mg tablets£8.99 – £31.99
Tadalafil 10mg tablets£8.99 – £31.99 -
 Tadalafil 5mg tablets£17.99 – £45.99
Tadalafil 5mg tablets£17.99 – £45.99
Depression and low testosterone
Similarly, depression can also involve a quick prescription for an SSRI. Again, like erectile dysfunction, signs of low testosterone can mimic depression.
Don’t blame your GP
The doctors working in the NHS are not at fault. They work within a “reactive” healthcare system that only responds when you get ill. This, coupled with the ten-minute consultation, doesn’t give the GP much opportunity to get to the heart of the issue.
Many GPs are not familiar with the subtle nuances of TRT. As mentioned above, many of the symptoms of hypogonadism match those of other conditions.
This lack of specialist knowledge is another reason GPs may be reluctant to initiate TRT. They would leave themselves exposed if they cannot manage a patient effectively and deal with adverse effects.
TRT and prostate cancer fears
The concerns regarding prostate cancer are another reason that many doctors are hesitant to begin TRT. However, the science behind the link between testosterone and prostate cancer is extremely weak and is based on studies stemming from 1941![6]
However, recent research has revealed that high testosterone levels do not increase prostate cancer risk [7,8].
BSSM Guidelines
It is not that there are no guidelines to follow. Current BSSM [9] guidelines provide clear information that would enable primary care doctors to help meet the needs of men suffering from late-onset hypogonadism. Unfortunately, despite this, the treatment protocols are still mired in the dark ages, with very few GPs willing to stick their heads over the parapet.
It will require a paradigm shift and the willingness of the “reactive” healthcare system to transform into a “proactive” healthcare system.
If your quest for the mythical NHS TRT has failed, do not despair. In the UK, TRT can be obtained privately from specialist TRT clinics. To start your TRT journey today, book your FREE initial TRT consultation with Medical Mojo, and we will point you in the right direction.
Disclaimer: This information is for educational purposes only and not a substitute for professional medical advice.
Are weight loss treatments making you tired, or have they led to a sudden increase in hair loss? Do you struggle with sleep?
Get a free month’s supply of one of our compounded treatments for energy, hair loss or sleep, with your first purchase of Mounjaro or Wegovy from Medical Mojo.
Claim your FREE offer
References:
- O’Connor DB, Archer J, Hair WM, Wu FC,”Exogenous testosterone, aggression, and mood in eugonadal and hypogonadal men” Physiol Behav, 2002Apr1, 75(4):557-66
- Hull University Teaching Hospitals NHS Trust. Amber list of Drugs
- EL(91)127 “Responsibility for Prescribing between Hospitals and GPs.”, DH
- Basil N. Late-onsethypogonadism. Med Clin North Am 2011; 95(3):507-523
- Mulligan T, Frick MF, Zuraw QC, et al. Prevalance of hypogonadism in males aged at least 45 years. The HIM study. Intl J Clin Pract 2000,(7);762-9
- Huggins, C., Stevens, R.E. and Hodges, C.V., 1941. Studies on prostatic cancer: II. The effects of castration on advanced carcinoma of the prostate gland. Archives of surgery, 43(2), pp.209-223.
- Morgentaler A. Testosterone replacement therapy and prostate cancer. Urol Clin NA 2007;34:555–63.
- Morgentaler A, Traish AM. Shifting the paradigm of testosterone and prostate cancer: the Saturation Model and the limits of androgendependent growth. Eur Urol 2009;55:310–21
- Hackett G, Kirby M, Rees RW, Jones TH, Muneer A, Livingston M, Ossei-Gerning N, David J, Foster J, Kalra PA, Ramachandran S. The British Society for Sexual Medicine Guidelines on Male Adult Testosterone Deficiency, with Statements for Practice. World J Mens Health. 2023 Jul;41(3):508-537.