Long COVID and coenzyme Q10 have become hot topics as many people continue to experience lingering symptoms long after recovering from COVID-19. Long COVID is characterised by ongoing fatigue, muscle pain, brain fog, and sleep problems that can last for months or even years. Recent research suggests that these persistent issues may be linked to mitochondrial dysfunction—the cells’ energy producers—which leads to low energy and increased inflammation. Can coenzyme Q10 help with the symptoms of long COVID?
-
 CoEnzyme Q10 50mg Soluble Oral PatchPrice range: £29.99 through £249.99
CoEnzyme Q10 50mg Soluble Oral PatchPrice range: £29.99 through £249.99 -
 Melatonin 8.5mg soluble oral patchPrice range: £35.99 through £99.99
Melatonin 8.5mg soluble oral patchPrice range: £35.99 through £99.99 -
 Low Dose Naltrexone 4.5mg Soluble Oral PatchPrice range: £39.99 through £124.99
Low Dose Naltrexone 4.5mg Soluble Oral PatchPrice range: £39.99 through £124.99
Coenzyme Q10 and long COVID in under a minute
Coenzyme Q10 (CoQ10) is a natural antioxidant that plays a crucial role in energy production within the mitochondria. For those dealing with long COVID, coenzyme Q10 might help boost energy levels and reduce inflammation, potentially easing symptoms such as fatigue and muscle pain.
Barletta M et al. [6] studied 174 chronic COVID syndrome patients, with 116 receiving coenzyme Q10 and alpha?lipoic acid and 58 receiving no treatment. They measured fatigue using the Fatigue Severity Scale (FSS).
The treatment group showed much better results—with 53.5% achieving a complete FSS response versus only 3.5% in the control group, making this the first promising study on these supplements for chronic COVID syndrome.
If you’re looking for effective ways to combat the challenges of long COVID, understanding the benefits of coenzyme Q10 might offer a new approach to recovery. Keep reading to learn more about coenzyme Q10 and long COVID and how they might help you return to feeling like yourself again.
COVID-19 and long COVID
SARS-CoV-2, the virus behind COVID-19, was first found in China in December 2019. According to the report from the World Health Organization (WHO), as of July 19, 2023, there have been 768,237,788 confirmed cases of COVID-19, and 6,951,677 of them have died. As of July 10, 2023, a total of 13,474,267,147 doses of vaccine have been administered [1].
COVID-19 can range from having no symptoms at all to causing life-threatening illness [2]. Even after recovery, some people develop long COVID.
In this condition, symptoms like fatigue, muscle pain, depression, sleep problems, memory loss, chest and joint pain, palpitations, and digestive issues continue for months.
This chronic post-viral syndrome, sometimes called “Long COVID,” affects many people, regardless of how severe their initial illness was [3].
COVID definitions
Recently, The National Institute for Health and Care Excellence (NICE) defined the stages of SARS-CoV-2 disease in relation to the time of onset of symptoms [3] and proposed the following definition:
- Acute COVID-19 infection: Signs and symptoms of COVID-19 for up to 4 weeks [3].
- Symptomatic COVID-19: Signs and symptoms of COVID-19 from 4 to 12 weeks not explained by an alternative diagnosis [3].
- Post-COVID-19 syndrome: Signs and symptoms that develop during or following an infection consistent with COVID-19, continue for?>?12 weeks and are not explained by an alternative diagnosis [3].
What causes long COVID?
Researchers believe that long COVID may be linked to ongoing inflammation caused by the body’s response to the virus.
When SARS?CoV?2 enters cells through a receptor called ACE?2 (found in many organs) [4], it triggers an immune response that can lead to a “cytokine storm,” an overproduction of inflammatory chemicals [5].
Mitochondria are responsible for providing energy to cells. Inflammation from COVID-19 can lower the production of ATP, the cell’s energy currency [6].
Mitochondrial dysfunction and long COVID
Mitochondria are essential for producing energy in cells, and inflammation from COVID-19 can reduce this energy production, causing fatigue and other issues.
Many studies show that problems with mitochondria—the cell’s energy producers—significantly affect the duration and severity of COVID-19 symptoms [9].
When mitochondria don’t work well or age, they create harmful oxygen radicals that damage cells, trigger too much inflammation, and even cause cell death.
Because of this, mitochondria are seen as key regulators of our immune system and inflammation. Research also suggests that improving mitochondrial function can help reduce inflammation and restore normal immune activity.
In COVID-19, faulty mitochondria may not only worsen the initial illness but also lead to long-lasting symptoms.
Who gets long COVID?
Some people who get infected with COVID develop long-lasting issues, known as long COVID, which can continue for many months.
In a study of 1733 COVID-19 survivors from Wuhan with a median age of 57, a follow-up about 186 days after symptoms began found that 52% reported fatigue or muscle weakness, 26% had sleep difficulties, and 23% experienced anxiety or depression.
Patients who were more severely ill showed worse outcomes, with 56% of those in the most severe group having impaired lung function compared to 22% in the mild group; their odds of lung problems were 1.61 times higher for moderate cases and 4.60 times higher for severe cases.
In addition, neutralising antibody levels dropped significantly from the acute phase, and some patients developed reduced kidney function.
These results highlight the long-term impact of COVID-19, especially in patients with severe initial illness, and emphasise the need for targeted long-term recovery strategies [7].
The similarities between long COVID and chronic fatigue syndrome
Long COVID shares many similarities with chronic fatigue syndrome ( also called myalgic encephalomyelitis), a condition that can follow other infections like SARS or Epstein-Barr virus [8].
Chronic COVID syndrome causes long-lasting fatigue, muscle pain, depression, and sleep problems—similar to conditions like chronic fatigue syndrome and fibromyalgia.
The key difference is that chronic fatigue syndrome is diagnosed only when symptoms persist for at least six months, while the full duration of long COVID is still unknown.
Coenzyme Q10 and chronic fatigue syndrome
Some nutrients that support the cell’s energy centres (mitochondria) have antioxidant effects, which may help reduce these symptoms.
In a study of 207 chronic fatigue syndrome patients, some received 200 mg of CoQ10 and 20 mg of NADH daily for 3 months, while others got a placebo.
Compared to those on the placebo, those taking the supplements reported much less fatigue, better overall quality of life, and improved sleep quality [10].
Nutrients for mitochondrial dysfunction and long COVID
Many studies show that inflammation decreases when mitochondria are renewed more effectively, and the immune system functions better [11].
Mitochondrial nutrients (MNs), like CoQ10 and alpha-lipoic acid (ALA), are known for their anti-inflammatory effects. When included in the diet, they help stop the uncontrolled production of harmful molecules called mitochondrial reactive oxygen species (mtROS), which can damage the mitochondria and cause problems for the body [12].
What is Coenzyme Q10?
Coenzyme Q10, or ubiquinone, is vital to the cell’s energy system and helps control gene activity. We also get CoQ10 from our diet.
During illnesses, both short-term and long-term, levels of CoQ10 can drop, leading to lower energy production and more free radicals. That’s why CoQ10 is used as a supplement in clinical practice—it is safe and has few side effects [13].
Research by Cordero and colleagues shows that fibromyalgia involves activating an inflammasome—a complex that triggers inflammation—and releasing inflammatory substances. This happens when CoQ10 levels are low; taking CoQ10 orally can help reduce this inflammation [14].
How the body produces energy
At this point, it might be a good idea to review how energy is made in the body.
Think of mitochondria as the body’s power stations. Instead of producing electricity, they make ATP, the energy currency that powers your cells.
Imagine the inner membranes of mitochondria as hundreds of tiny hydroelectric plants. To add to the picture, mitochondria have an outer and inner membrane surrounding an area called the matrix. Check out the diagram below for a clearer view.
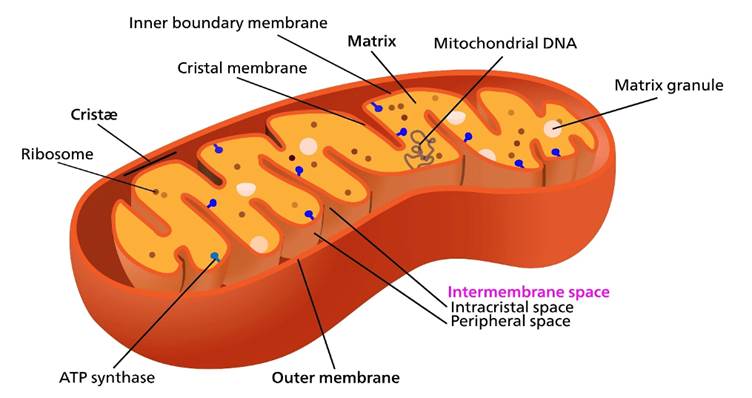
I’m assuming you know how hydroelectric dams work, but here’s a quick refresher if you need one. Imagine a reservoir high on a mountain where a dam holds back water. When the water is released, it flows downhill due to gravity, turning turbines to produce electricity.
Now, picture replacing the water with protons and the turbines with ATPase—this is how your body creates energy. ATPase is the tiniest machine known, and it spins like a turbine. If there aren’t enough “buckets” to fill the reservoir, there’s no water to turn the turbines, and energy production stops. In your body, lacking CoQ10 means there’s little or no energy.
How does CoQ10 make energy in the body?
Coenzyme Q10 is the compound that shuttles electrons from Complex I (or II) to Complex III in the electron transport chain within the cell’s powerhouses, the mitochondria [15].
The shuttling of electrons across the electron transport chain provides the energy to push protons to the outside of the inner membrane of the mitochondria.
This then creates a proton gradient with respect to the inside (remember the analogy of the hydroelectric dam above), allowing the protons to flow back inside the matrix via the ATPase, creating energy in the form of ATP [16].
In addition to being a shuttle for the electrons, CoQ10 has a vital role as an antioxidant. This is because if the electrons can’t be carried from Complex to Complex in an organised fashion, they’ll leak out into the inner matrix of the mitochondria and wreak havoc as free radicals [17].
Coenzyme Q10?+?alpha lipoic acid for chronic COVID syndrome
Many studies suggest that improving mitochondrial function can help reduce inflammation and restore the immune system. In COVID-19, mitochondrial problems might worsen the symptoms and contribute to the disease becoming chronic.
Some studies suggest that certain nutrients with antioxidant and anti-inflammatory properties, like coenzyme Q10 (CoQ10) and alpha?lipoic acid (ALA), might help.
CoQ10 is a natural part of the cell’s energy system and helps control inflammation, while ALA is a strong antioxidant that supports energy production and can calm inflammation.
Recent research has even shown that combining coenzyme Q10 and ALA may boost energy production and reduce oxidative stress (damage caused by harmful molecules) in cells.
CoQ10 and alpha-lipoic acid improves symptoms of fatigue
Barletta M et al. [6] studied the effect of supplementing coenzyme Q10 and alpha-lipoic acid in 174 patients with chronic COVID syndrome, who were split into two groups.
One group (116 patients) took coenzyme Q10 and alpha?lipoic acid, while the other group (58 patients) received no treatment. The results were measured by measuring fatigue using the Fatigue Severity Scale (FSS) [6].
The treatment group showed much better results. A complete response on the FSS was seen in 62 patients (53.5%) in the treatment group, compared to only two patients (3.5%) in the control group.
Also, only 9.5% of the treatment group had less than a 20% reduction in fatigue, while 25.9% of the control group showed such a low response [6].
This is the first study to test coenzyme Q10 and alpha?lipoic acid for chronic COVID syndrome, and the results are promising [6].
Coenzyme Q10 for long COVID
If you are interested in supplementing your diet with coenzyme Q10 to help with the symptoms of long COVID, then there are a few things to bear in mind.
Despite being an amazing supplement that we believe everyone should be taking, coenzyme Q10 has an issue with absorption. It is notoriously difficult to get into the bloodstream after being taken orally, so we may not be getting all of its benefits.
To get around the issue of CoQ10’s poor absorption, Medical Mojo has teamed up with APC labs to develop a buccal or soluble oral patch that bypasses the stomach and delivers the drug straight into the bloodstream. Read the following section to learn more about the benefits of buccal absorption.
Buccal Drug Delivery of CoQ10
The CoQ10-soluble oral patch is placed on the inside of your cheek, where it then dissolves. This method bypasses the stomach and intestines, delivering CoQ10 directly into the bloodstream for faster and more efficient absorption—kind of like a VIP pass straight into your circulation! This means more CoQ10 is absorbed, and less is wasted.
Check out our range of patches to learn more about the Medical Mojo CoQ10 50mg soluble oral patch, and watch the video below for instructions on how to use it.
FREE long COVID consultation
If you have long COVID and are unsure what steps to take, book a FREE consultation with one of our prescribers. They will guide you to the best evidence-based treatments and can even recommend bespoke compounded solutions.
To get in touch, email info@medicalmojo.co.uk or call 023 8157 5111
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice.
Get medicines tailored to you
Our compounding service gives you treatment built around your unique needs.
Learn moreReferences:
- Yousefi, R. and Mokaramian, S., 2024. An Overview of the Infection, Mortality, and Vaccination Statistics of Covid-19 from the Beginning Until July 19. Eurasian Journal of Science and Technology, 4(3).
- Kim, G.U., Kim, M.J., Ra, S.H., Lee, J., Bae, S., Jung, J. and Kim, S.H., 2020. Clinical characteristics of asymptomatic and symptomatic patients with mild COVID-19. Clinical microbiology and infection, 26(7), pp.948-e1.https://www.sciencedirect.com/science/article/pii/S1198743X20302688
- Carfì, A., Bernabei, R. and Landi, F., 2020. Persistent symptoms in patients after acute COVID-19. Jama, 324(6), pp.603-605.
- Yan, Z., Yang, M. and Lai, C.L., 2021. Long COVID-19 syndrome: a comprehensive review of its effect on various organ systems and recommendation on rehabilitation plans. Biomedicines, 9(8), p.966.
- Hu, B., Huang, S. and Yin, L., 2021. The cytokine storm and COVID?19. Journal of medical virology, 93(1), pp.250-256.
- Barletta, M.A., Marino, G., Spagnolo, B. et al. Coenzyme Q10?+?alpha lipoic acid for chronic COVID syndrome. Clin Exp Med 23, 667–678 (2023).
- Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, Kang L, Guo L, Liu M, Zhou X, Luo J, Huang Z, Tu S, Zhao Y, Chen L, Xu D, Li Y, Li C, Peng L, Li Y, Xie W, Cui D, Shang L, Fan G, Xu J, Wang G, Wang Y, Zhong J, Wang C, Wang J, Zhang D, Cao B. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2023 Jun 17;401(10393)
- Jones, J.F., Ray, C.G., Minnich, L.L., HICKS, M.J., KIBLER, R. and LUCAS, D.O., 1985. Evidence for active Epstein-Barr virus infection in patients with persistent, unexplained illnesses: elevated anti-early antigen antibodies. Annals of internal medicine, 102(1), pp.1-7.
- Fernández-Ayala, D.J.M., Navas, P. and López-Lluch, G., 2020. Age-related mitochondrial dysfunction as a key factor in COVID-19 disease. Experimental gerontology, 142, p.111147.
- Castro-Marrero, J., Segundo, M.J., Lacasa, M., Martinez-Martinez, A., Sentañes, R.S. and Alegre-Martin, J., 2021. Effect of dietary coenzyme Q10 plus NADH supplementation on fatigue perception and health-related quality of life in individuals with myalgic encephalomyelitis/chronic fatigue syndrome: a prospective, randomized, double-blind, placebo-controlled trial. Nutrients, 13(8), p.2658.
- Missiroli, S., Genovese, I., Perrone, M., Vezzani, B., Vitto, V.A. and Giorgi, C., 2020. The role of mitochondria in inflammation: from cancer to neurodegenerative disorders. Journal of clinical medicine, 9(3), p.740.
- Fan, L., Feng, Y., Chen, G.C., Qin, L.Q., Fu, C.L. and Chen, L.H., 2017. Effects of coenzyme Q10 supplementation on inflammatory markers: A systematic review and meta-analysis of randomized controlled trials. Pharmacological research, 119, pp.128-136.
- Crane, F.L., 2001. Biochemical functions of coenzyme Q10. Journal of the American College of Nutrition, 20(6), pp.591-598.
- Cordero MD, Alcocer-Gómez E, de Miguel M, Culic O, Carrión AM, Alvarez-Suarez JM, Bullón P, Battino M, Fernández-Rodríguez A, Sánchez-Alcazar JA. Can coenzyme q10 improve clinical and molecular parameters in fibromyalgia? Antioxid Redox Signal. 2013 Oct 20;19(12):1356-61.
- Casagrande, D., Waib, P.H. and Júnior, A.A.J., 2018. Mechanisms of action and effects of the administration of Coenzyme Q10 on metabolic syndrome. Journal of Nutrition & Intermediary Metabolism, 13, pp.26-32.
- Cogliati, S., Cabrera-Alarcón, J.L. and Enriquez, J.A., 2021. Regulation and functional role of the electron transport chain supercomplexes. Biochemical Society Transactions, 49(6), pp.2655-2668.
- Bentinger, M., Brismar, K. and Dallner, G., 2007. The antioxidant role of coenzyme Q. Mitochondrion, 7, pp.S41-S50.